Poster ID: FRI-267, EASL Congress 2024
ABSTRACT
Authors: Dan-Qin Sun1,2,3, Jia-Qi Shen1,2,3, Xiao-Fei Tong4, Yangyang LI5, Giovanni Targher6, Yayun Ren7, Haiyang Yuan8, Chris D Byrne9, Hong You4, Ming-Hua Zheng8,10
1. Urologic Nephrology Center, Jiangnan University Medical Center, Wuxi, China
2. Affiliated Wuxi Clinical College of Nantong University, Wuxi, China
3. Wuxi No.2 People’s Hospital, Wuxi, China
4, Liver Research Center, Beijing Friendship Hospital, Beijing Key Laboratory of Translational Medicine on Liver Cirrhosis, National Clinical Research Center of Digestive Diseases, Capital Medical University, Beijing, China
5. Key Laboratory of Diagnosis and Treatment for the Development of Chronic Liver Disease in Zhejiang Province, Wenzhou, China
6. Section of Endocrinology, Diabetes and Metabolism, Department of Medicine, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy
7. Choutu Technology, Zhejiang, China
8. MAFLD Research Center, Department of Hepatology, the First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
9. Southampton National Institute for Health and Care Research Biomedical Research Centre, University Hospital Southampton and University of Southampton, Southampton General Hospital, Southampton, United Kingdom
10. Key Laboratory of Diagnosis and Treatment for The Development of Chronic Liver Disease in Zhejiang Province, Wenzhou, China
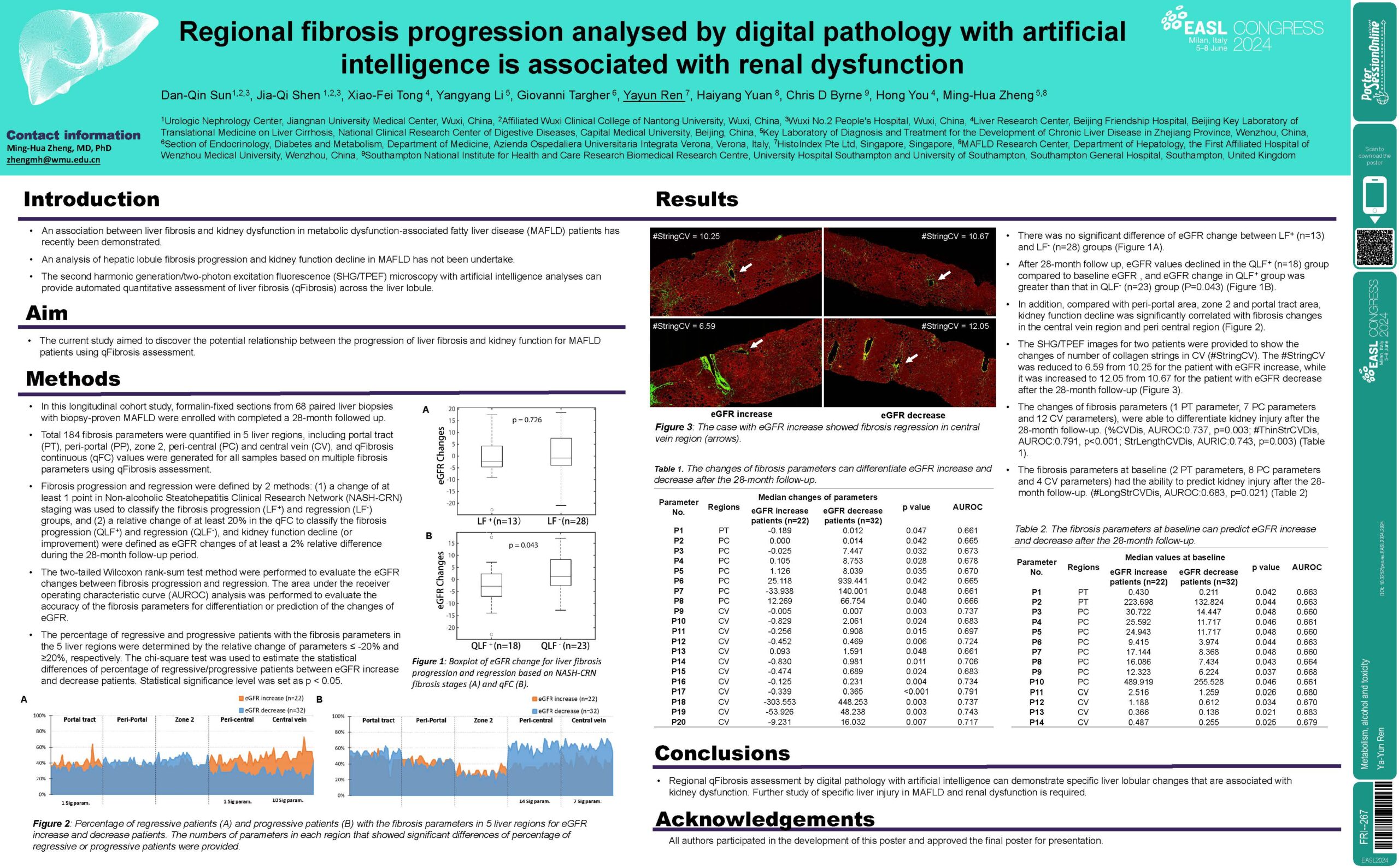
Background and Aims: An association between liver fibrosis and kidney dysfunction in metabolic dysfunction-associated fatty liver disease (MAFLD) patients has recently been demonstrated. However, an analysis of hepatic lobule fibrosis progression and kidney function decline in MAFLD has not been undertake. The second harmonic generation/two-photon excitation fluorescence (SHG/TPEF) microscopy with artificial intelligence analyses can provide automated quantitative assessment of liver fibrosis (qFibrosis) across the liver lobule. In this study, we aimed to discover the potential relationship between the progression of liver fibrosis and kidney function for MAFLD patients using qFibrosis assessment.
Method: In this longitudinal cohort study, formalin-fixed sections from 58 paired liver biopsies were enrolled with completed a 28 month followed up. Total 184 fibrosis parameters were quantified in 5 liver regions, including portal tract (PT), peri-portal (PP), zone 2, peri-central (PC) and central vein (CV), and qFibrosis continuous (qFC) values were generated for all samples based on 10 fibrosis parameters using qFibrosis assessment. Liver fibrosis progression (LF+) and regression (LF-) was defined as qFC changes of at least a 20% relative difference, and kidney function decline (or improvement) were defined as eGFR changes of at least a 2% relative difference during the 28-month follow-up period. The two-tailed Wilcoxon rank-sum test and the Spearman nonparametric method were performed to test the independence of associations between liver fibrosis and eGFR.
Results: There was no significant difference in liver fibrosis stage and eGFR at the first and second liver biopsy. However, after 28 month follow up, eGFR values declined in the LF+ group compared to baseline eGFR. Moreover, eGFR change in LF+ group evaluated by qFibrosis was greater than that in LF- group (P=0.043). In addition, compared with peri-portal area, zone 2 and portal tract area, kidney function decline was significantly correlated with fibrosis changes in the central vein region and peri- central region. Regional qFibrosis parameters were also able to differentiate kidney injury (%CVDis, AUC:0.737, P=0.003; #ThinStrCVDis, AUC:0.791, P=0.000; StrLengthCVDis, AUC:0.743, P=0.003).
Conclusion: Regional qFibrosis assessment by digital pathology with artificial intelligence can demonstrate specific liver lobular changes that are associated with kidney dysfunction. Further study of specific liver injury in MAFLD and renal dysfunction is required.