Poster ID: TOP-310, EASL Congress 2024
ABSTRACT
Title: Genetic determinants of disease progression in metabolic dysfunction-associated liver disease patients unresponsive to lifestyle intervention: implications for personalized medicine
Authors: Aruhan Yang1, Xiaoxue Zhu1, Qiang Yang2, Xiao Teng3, Yanhua Ding4
1. Phase One Clinical Research Center, First Hospital of Jilin university, Changchun, China
2. Hangzhou Choutu Technology Co., Ltd., hangzhou, China
3. HistoIndex Pte Ltd, Singapore, Singapore, Singapore
4. Phase One Clinical Research Center, First Hospital of Jilin university, Changchun, China
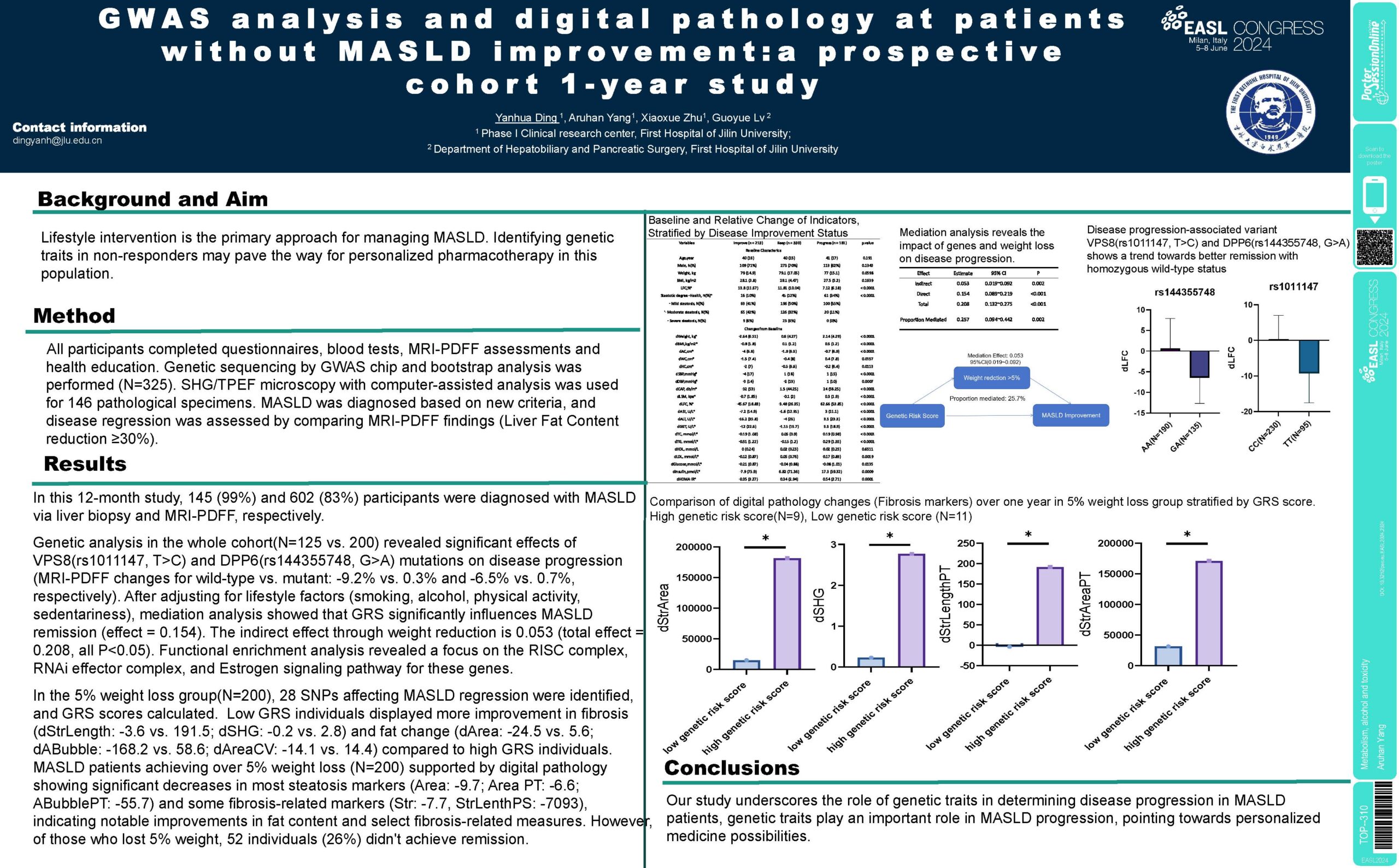
Background and Aims: Lifestyle intervention with 5% weight loss (WL) is the primary approach for managing MASLD. Identifying genetic traits in non-responders may pave the way for personalized pharmacotherapy in this population.
Method: In this study with 724 participants, 146 had liver biopsies. All participants completed questionnaires, blood tests, and MRI PDFF assessments. Genetic sequencing was performed on collected blood samples, and SHG/TPEF microscopy with computer-assisted analysis was used for pathological specimens. Patients with liver biopsies received lifestyle interventions, while others received health education. MASLD was diagnosed based on new criteria, and disease regression was assessed by comparing two sets of pathological (NAS reduction ≥ 2 points) or MRI findings (Liver Fat Content, LFC reduction ≥ 30%).
Results: In this 12-month study, 145 (99%) and 602 (83%) participants were diagnosed with MASLD via liver biopsy and MRI-PDFF, respectively. In individuals achieving MASLD remission(N = 213, 35.3%), significant improvements in liver damage markers (ALT, AST, GGT) and metabolic parameters (Glucose, Insulin, HOMA, LDL, TG) were observed, highlighting enhanced hepatic health and glucose lipid metabolism.
Genetic analysis in the whole cohort revealed significant effects of VPS8(rs1011147, T > C) and DPP6(rs144355748, G > A) mutations on disease progression (LFC changes for wild-type vs. mutant: – 9.2% vs. 0.3% and – 6.5% vs. 0.7%, respectively). After adjusting for lifestyle factors (smoking, alcohol, physical activity, sedentariness), mediation analysis found 25% of the gene’s effect on improving MASLD was indirectly mediated through WL > 5%, while the remaining 75% represents the direct influence of the gene independent of WL > 5%.
MASLD patients achieving over 5% WL (N = 200) showed an average 34% LFC reduction and 2 points NAS reduction, supported by digital pathology showing significant decreases in most steatosis markers (Area: -9.7; Area PT: -6.6; ABubblePT: -55.7) and some fibrosis-related markers (Str: -7.7, StrLenthPS: -7093), indicating notable improvements in fat content and select fibrosis-related measures. However, 52 individuals with WL > 5% (26%) didn’t achieve remission. 28 SNPs affecting MASLD regression were identified among the WL > 5% group, and GRS scores calculated. Low GRS individuals displayed more improvement in fibrosis (dStrLength: -3.6 vs. 191.5; dSHG: -0.2 vs. 2.8) and steatosis (dArea: -24.5 vs. 5.6; dABubble: -168.2 vs. 58.6; dAreaCV: -14.1 vs. 14.4) compared to high GRS individuals. Functional enrichment analysis revealed a focus on the RISC complex, RNAi effector complex, and Estrogen signaling pathway for these genes.
Conclusion: Our study underscores the role of genetic traits in determining disease progression in MASLD patients resistant to 5% weight loss, pointing towards personalized medicine possibilities.