Poster ID: WED-319, EASL Congress 2024
ABSTRACT
Authors: Xiaoxue Zhu1, Aruhan Yang1, Wen Wang1, Hong Zhang1, Guoyue LV1, Yanhua Ding1, Qiang Yang2, Xiao Teng3
1. The First Hospital of Jilin University, Changchun, China,
2. Hangzhou Choutu Technology Co.Ltd., Hangzhou, China,
3. HistoIndex Pte Ltd, Singapore, Singapore
Background and Aims: At present, there is no medication approved for the treatment of metabolic dysfunction-associated steatotic liver disease (MASLD). Lifestyle interventions that result in weight loss are considered to offer some improvement in MASLD. Pathology serves as the benchmark for evaluating their effectiveness. This study aimed to assess the efficacy of lifestyle interventions in patients with MASLD with the help of AI digital pathology.
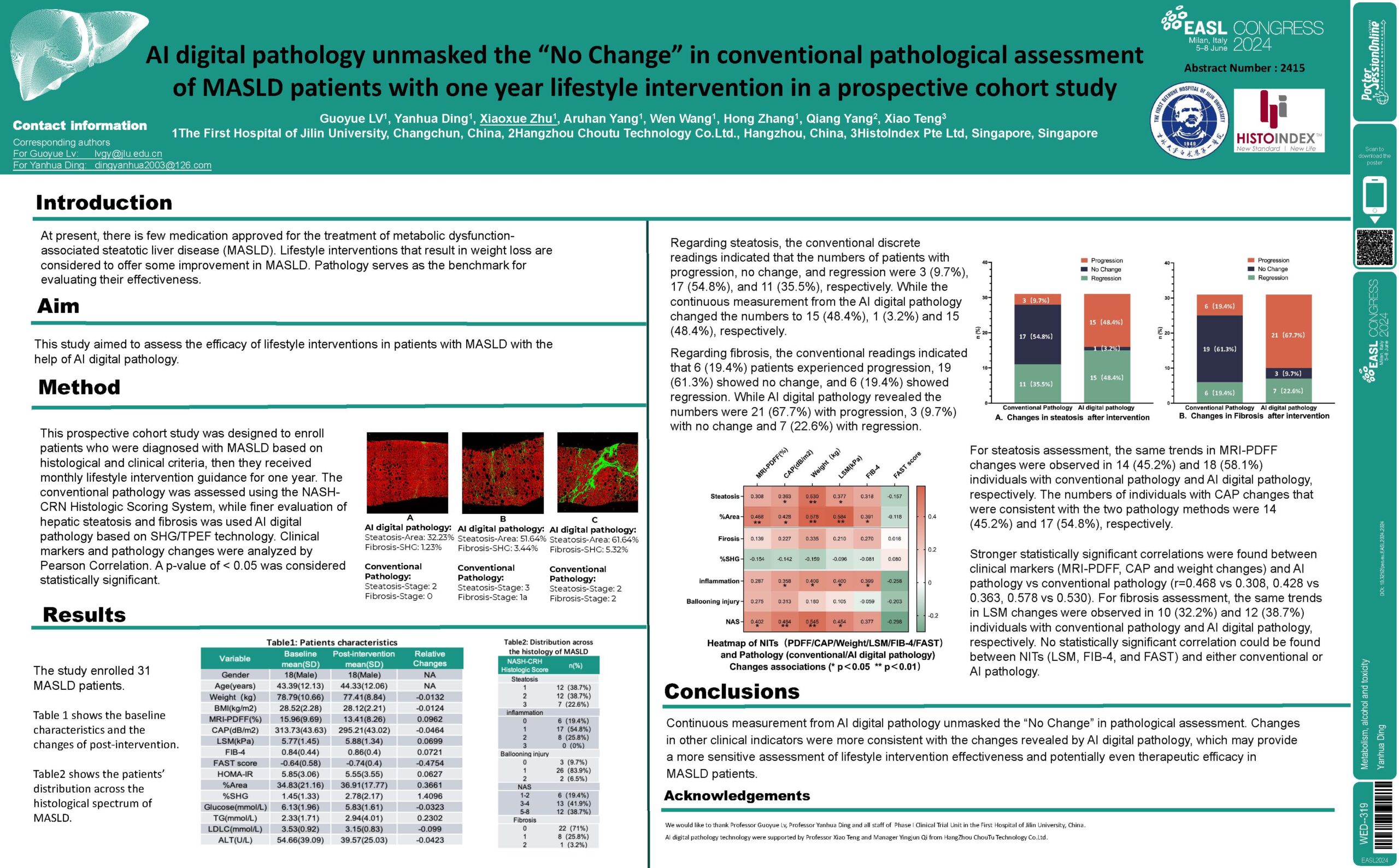
Method: This prospective cohort study involved 31 patients who were diagnosed with MASLD based on histological and clinical criteria, then they received monthly lifestyle intervention guidance for one year. The conventional pathology was assessed using the NASH-CRN Histologic Scoring System, while finer evaluation of hepatic steatosis and fibrosis was used AI digital pathology based on SHG/TPEF technology. Clinical markers and pathology changes were analyzed by Pearson Correlation. A p-value of < 0.05 was considered statistically significant.
Results: Regarding steatosis, the conventional discrete readings indicated that the numbers of patients with progression, no change, and regression were 3 (9.7%), 17 (54.8%), and 11 (35.5%), respectively. While the continuous measurement from the AI digital pathology changed the numbers to 15 (48.4%), 1 (3.2%) and 15 (48.4%), respectively. Regarding fibrosis, the conventional readings indicated that 6 (19.4%) patients experienced progression, 19 (61.3%) showed no change, and 6 (19.4%) showed regression. While AI digital pathology revealed the numbers were 21 (67.7%) with progression, 3 (9.7%) with no change and 7 (22.6%) with regression. For steatosis assessment, the same trends in MRI-PDFF changes were observed in 14 (45.2%) and 18 (58.1%) individuals with conventional pathology and AI digital pathology, respectively. The numbers of individuals with CAP changes that were consistent with the two pathology methods were 14 (45.2%) and 17 (54.8%), respectively. Stronger statistically significant correlations were found between clinical markers (MRI-PDFF, CAP and weight changes) and AI pathology vs conventional pathology (r=0.468 vs 0.308, 0.428 vs 0.363, 0.578 vs 0.530). For fibrosis assessment, the same trends in LSM changes were observed in 10 (32.2%) and 12 (38.7%) individuals with conventional pathology and AI digital pathology, respectively. No statistically significant correlation could be found between NITs (LSM, FIB-4, and FAST) and either conventional or AI pathology.
Conclusion: Continuous measurement from AI digital pathology unmasked the “No Change” in pathological assessment. Changes in other clinical indicators were more consistent with the changes revealed by AI digital pathology, which may provide a more sensitive assessment of lifestyle intervention effectiveness and potentially even therapeutic efficacy in MASLD patients