Introduction
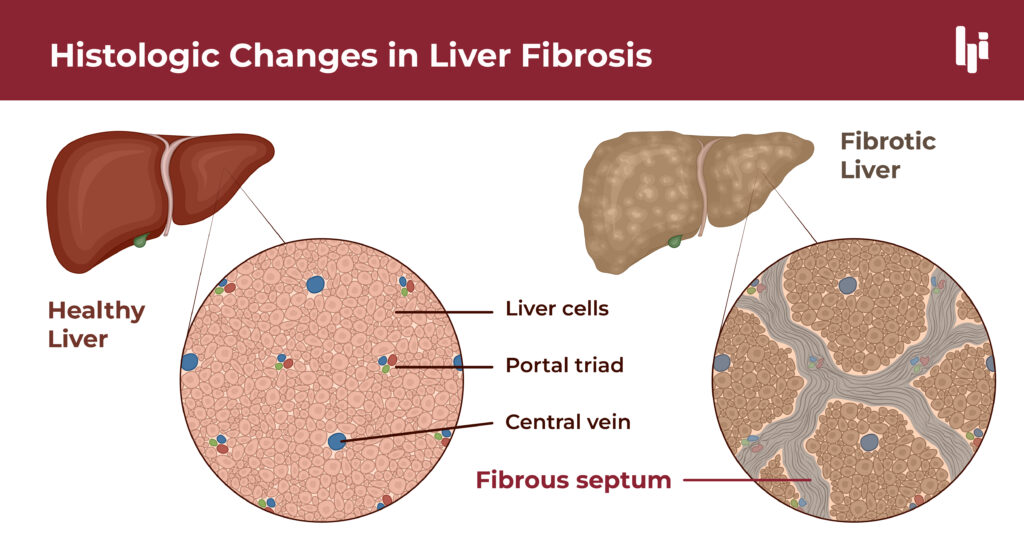
Liver fibrosis, a progressive scarring of the liver tissue, is a critical condition that often develops due to chronic liver diseases such as hepatitis, alcohol abuse, or Metabolic dysfunction–associated steatotic liver disease (MASLD). The progression of liver fibrosis can lead to poor patient outcomes like, cirrhosis and liver failure, making early detection and accurate diagnosis critical for effective treatment. With advancements in medical technology, particularly in imaging and AI, the landscape of liver fibrosis imaging and diagnosis is rapidly improving, offering new hope for patients and clinicians alike.
Understanding Liver Fibrosis
What is Liver Fibrosis?
Causes and Risk Factors
Traditional Diagnostic Methods
Biopsy Techniques
Liver fibrosis can be caused by a variety of factors, many of which are linked to chronic liver disease. The most common causes include:
- Viral Infections: Chronic hepatitis B and C infections are leading causes of liver fibrosis worldwide. The persistent viral infection triggers an ongoing inflammatory response, resulting in fibrosis5.
- Alcohol Abuse: Chronic and excessive alcohol consumption leads to alcoholic liver disease, which can progress to fibrosis as the liver struggles to repair the continuous damage caused by alcohol.
- Metabolic dysfunction–associated steatotic liver disease (MASLD): MASLD, particularly its more severe form known as Metabolic dysfunction-associated steatohepatitis (MASH), is a growing cause of liver fibrosis, driven by the global rise in obesity and metabolic syndrome8.
- Other Contributing Conditions: Conditions like Alpha-1 Antitrypsin Deficiency (AATD), biliary atresia (BA), primary sclerosing cholangitis (PSC), primary biliary cholangitis (PBC), autoimmune hepatitis (AIH), and viral hepatitis B and C are significant contributors to liver fibrosis.
Understanding these causes and risk factors is crucial for both prevention and early intervention, particularly as some forms of fibrosis are more aggressive and lead to quicker progression to cirrhosis.
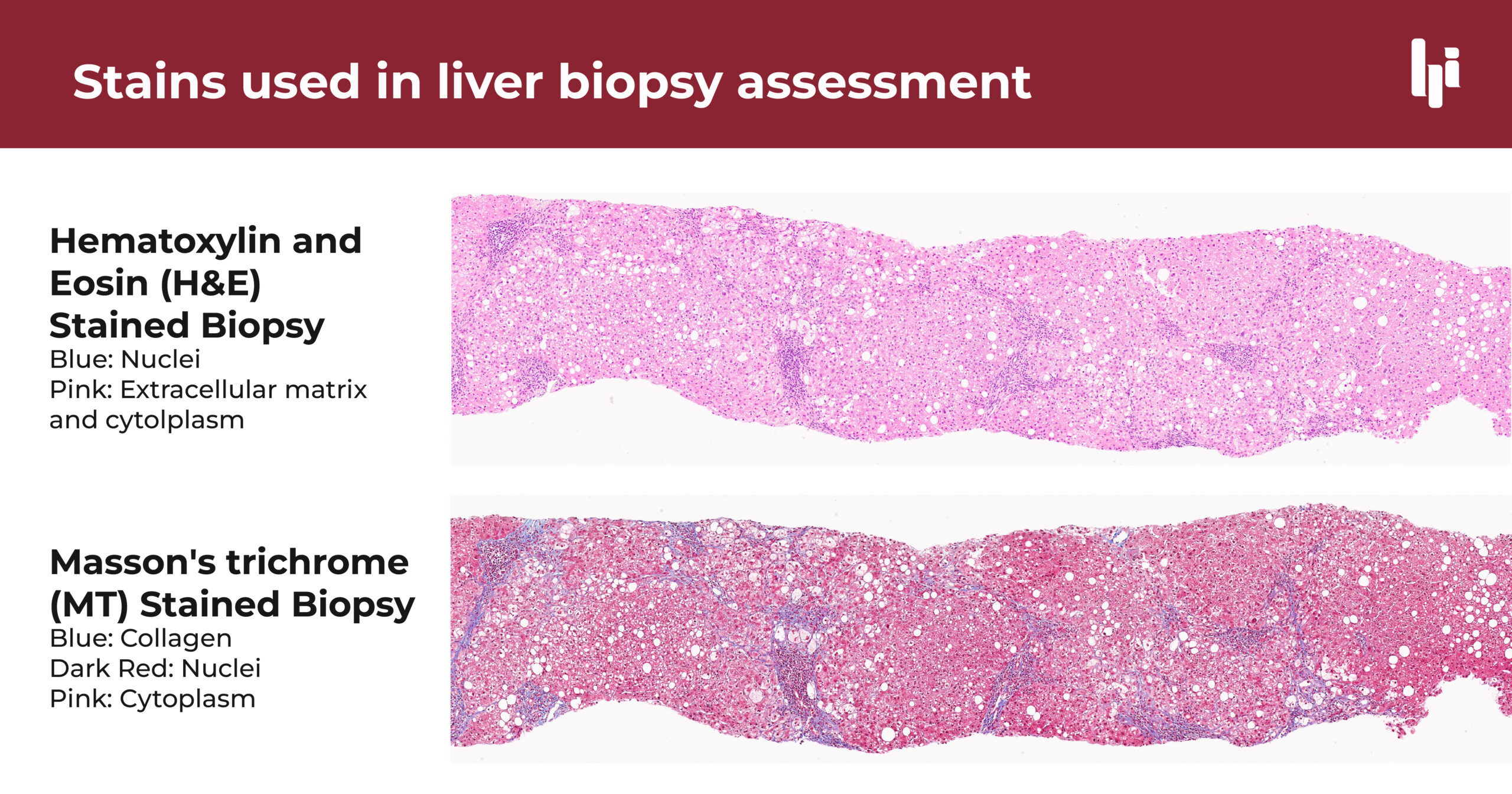
Liver biopsy has long been considered the gold standard for diagnosing liver fibrosis. The procedure involves extracting a small sample of liver tissue using a needle, which is then examined under a microscope for signs of fibrosis. While effective, liver biopsy is an invasive procedure associated with several risks, including pain, bleeding, and infection6. Additionally, the procedure’s sampling variability can sometimes result in inaccurate assessments, as fibrosis may not be evenly distributed throughout the liver.
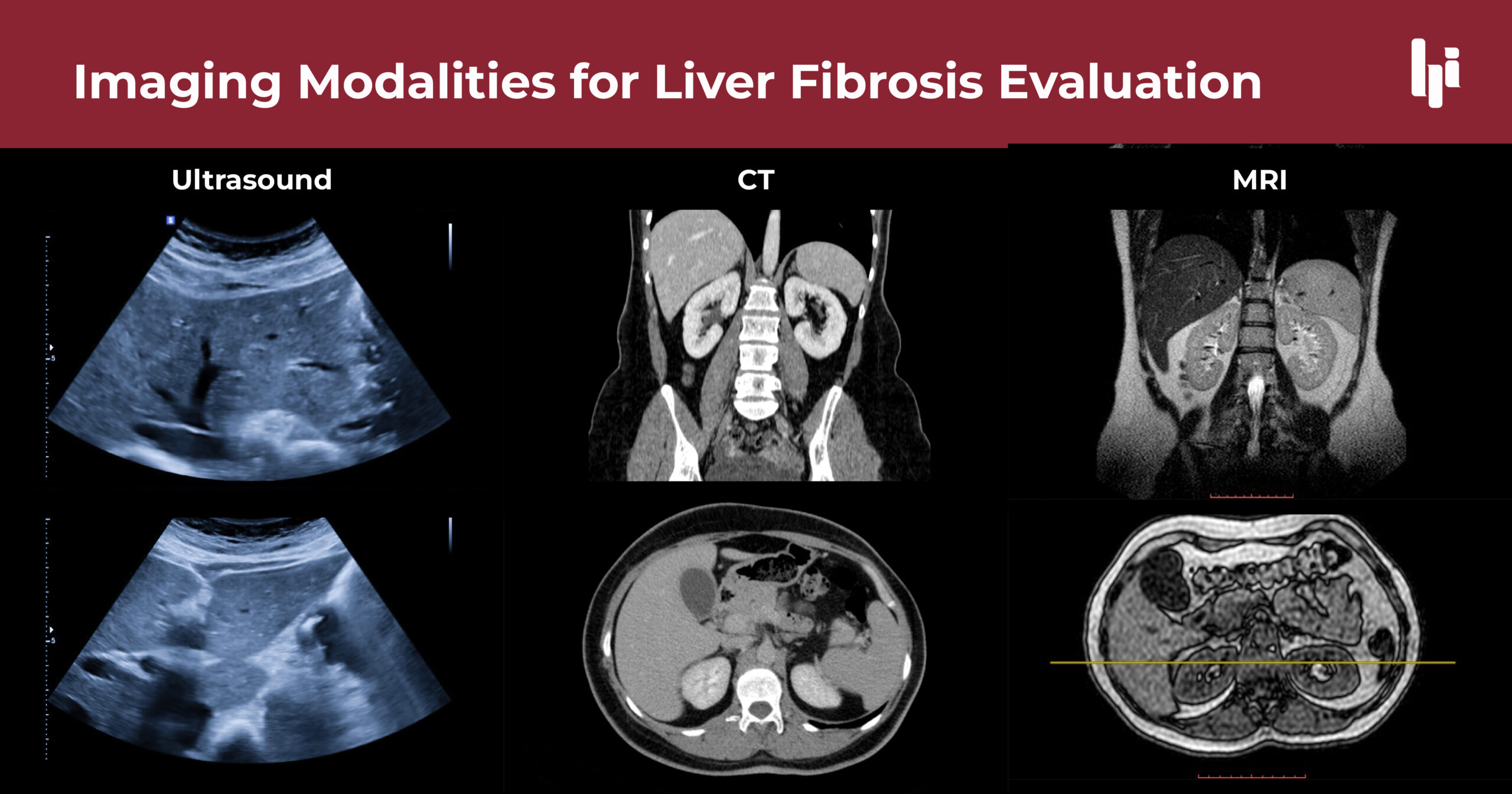
Imaging Modalities
Traditional imaging techniques, such as ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI), are often used to assess liver structure and detect the presence of fibrosis. However, these methods have limitations in detecting early-stage fibrosis due to their lower sensitivity. For example, while ultrasound is commonly used for liver examination of fat storage, inflammation, and swelling, its ability to detect mild fibrosis is limited. CT scans and MRI offer better resolution but are often unable to differentiate between mild and moderate fibrosis, making them less effective for early detection1.
Innovations in Liver Fibrosis Imaging
Advances in Non-Invasive Imaging Techniques
In recent years, there has been significant progress in developing non-invasive imaging techniques that can accurately assess liver fibrosis without the need for a biopsy. One such technique is elastography, which measures liver stiffness—a key indicator of fibrosis. Elastography can be performed using ultrasound-based methods (Transient Elastography, or TE) or MRI-based methods (Magnetic Resonance Elastography, or MRE). These technologies provide a non-invasive, reliable, and reproducible means of assessing liver fibrosis, offering a significant advantage over traditional methods4.
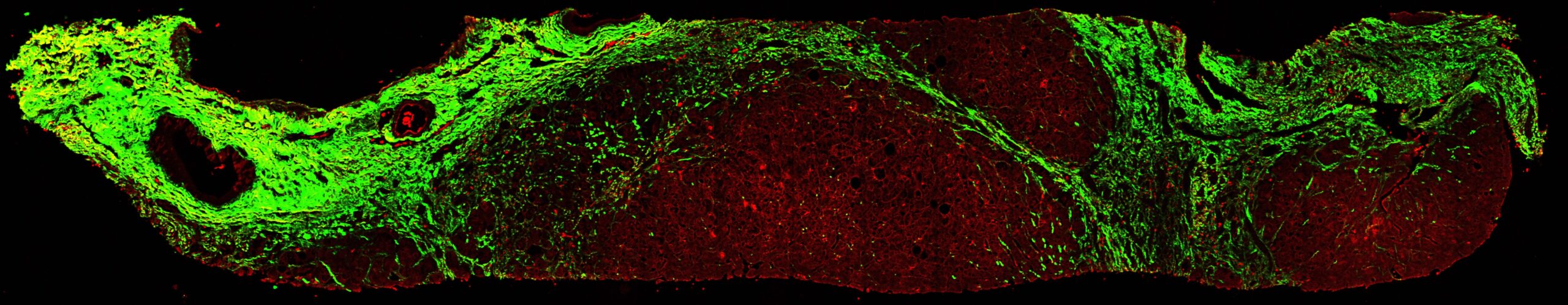
Second Harmonic Generation (SHG) Imaging
SHG imaging is a powerful tool in liver fibrosis assessment. Unlike traditional imaging methods, SHG imaging directly visualizes collagen fibers in liver tissue, offering a clear and detailed view of fibrosis. This high level of detail is critical for accurately assessing the extent and severity of fibrosis, particularly in early-stage disease. Moreover, SHG is non-destructive and can be performed on unstained tissue samples, preserving the integrity of the specimen for further analysis3.
AI-Powered Imaging Solutions
Benefits of Modern Imaging Technologies
The advancements in liver fibrosis imaging technologies offer several benefits:
- Greater Accuracy: Non-invasive imaging techniques, particularly when combined with AI, provide more accurate assessments of liver fibrosis, even in its early stages.
- Reduced Risk: Unlike biopsies, these imaging methods are non-invasive, eliminating the risks associated with tissue sampling.
- Improved Patient Comfort: Patients experience less discomfort and anxiety with non-invasive imaging compared to invasive procedures like biopsies.
These benefits not only improve diagnostic outcomes but also enhance the overall patient experience, making regular monitoring more feasible.
Clinical Applications
Improving Diagnosis Accuracy
The use of a combination of these techniques can improve the accuracy of liver fibrosis diagnosis, particularly in complex cases where traditional methods fall short. For instance, when non-invasive test modalities are discordant—where different tests provide conflicting results—additional testing via liver biopsies offer additional information and critical insights. The detailed and precise assessment of liver tissue using these technologies can help clinicians make more informed decisions, ultimately leading to better patient outcomes.
Enhancing Treatment Plans
Accurate imaging is not only crucial for diagnosis but also for guiding treatment. With detailed and precise assessments of fibrosis, clinicians can tailor treatment plans to the individual needs of each patient, ensuring that interventions are appropriate and effective. This personalized approach improves overall care and has the potential to slow or even reverse the progression of liver fibrosis.
Deepening Disease Understanding
The use of multi-modal imaging techniques that combine the strengths of different methods, such as elastography with SHG imaging, has provided a more comprehensive assessment of liver health. The inclusion of AI and machine learning is expected to deepen our understanding of fibrosis processes, especially the differences in progression and regression dynamics. These insights can improve the way fibrosis severity is assessed, and allow the development of tests or treatments that target specific mechanisms driving fibrosis.
Histoindex's Cutting-Edge Liver Fibrosis Imaging Solution
HistoIndex is at the forefront of innovation in liver fibrosis imaging, offering advanced imaging solutions powered by AI. The Genesis® Imaging System utilizes SHG imaging, a technique that provides high-resolution, detailed images of liver tissue without the need for staining or chemical alterations. The integration of AI analyzes the detailed images produced by SHG, providing an objective and quantifiable assessment of fibrosis. This approach reduces the subjectivity and variability often associated with manual image interpretation, leading to more consistent and accurate diagnoses.
FAQs
Liver fibrosis is the progressive scarring of the liver tissue due to chronic liver injury or inflammation.
Common causes include viral infections (hepatitis B and C), alcohol abuse, and non-alcoholic fatty liver disease (NAFLD).
Diagnosis is typically made through a combination of liver biopsy, imaging techniques, and non-invasive tests.
Early stages of liver fibrosis often have no symptoms; however, advanced stages can lead to symptoms such as jaundice, fatigue, and abdominal pain.
Traditional methods include liver biopsy, ultrasound, CT scans, and MRI.
Techniques like elastography measure liver stiffness, which correlates with fibrosis severity.
AI enhances accuracy, reduces variability in diagnosis, and provides more detailed analysis of imaging data.
SHG is an imaging technique that visualizes collagen fibers in liver tissue, providing detailed images crucial for fibrosis assessment.
HistoIndex uses AI algorithms to analyze SHG imaging images, improving diagnostic accuracy and consistency.
Future advancements may include multi-modal imaging techniques and real-time AI analysis, further enhancing diagnostic capabilities.
References
- Barr, Richard G., et al. “Elastography Assessment of Liver Fibrosis: Society of Radiologists in Ultrasound Consensus Conference Statement.” Radiology, vol. 276, no. 3, 2015, pp. 845-861.
- Bataller, Ramón, and David A. Brenner. “Liver Fibrosis.” Journal of Clinical Investigation, vol. 115, no. 2, 2005, pp. 209-218.
- Campagnola, Paul J., and Leslie M. Loew. “Second-Harmonic Imaging Microscopy for Visualizing Biomolecular Arrays in Cells, Tissues, and Organisms.” Nature Biotechnology, vol. 21, no. 11, 2003, pp. 1356-1360.
- Castera, Laurent, et al. “Non-Invasive Evaluation of Liver Fibrosis Using Transient Elastography.” Journal of Hepatology, vol. 48, no. 5, 2008, pp. 835-847.
- Friedman, Scott L. “Liver Fibrosis—From Bench to Bedside.” Journal of Hepatology, vol. 38, no. 1, 2003, pp. S38-S53.
- Rockey, Don C., et al. “Liver Biopsy.” Hepatology, vol. 49, no. 3, 2009, pp. 1017-1044.
- Yasaka, Koji, et al. “Deep Learning with Convolutional Neural Network for Differentiation of Liver Masses at Dynamic Contrast-Enhanced CT: A Preliminary Study.” Radiology, vol. 286, no. 3, 2018, pp. 887-896.
- Younossi, Zobair M., et al. “Global Epidemiology of Nonalcoholic Fatty Liver Disease—Meta‐Analytic Assessment of Prevalence, Incidence, and Outcomes.” Hepatology, vol. 64, no. 1, 2016, pp.